Glaucoma, often called the ‘Silent Thief of Sight,’ often develops gradually without immediate symptoms. It is a chronic, progressive disease in which the major nerve of the eye, the optic nerve, is permanently damaged. Major risk factors include elevated eye pressure, family history, age, low blood pressure and a thin cornea.
Over 80 million people around the world have glaucoma and it is one of the leading causes of blindness and visual impairment in the United States today. It is estimated that over four million people have glaucoma in the U.S. but only half of them know it. The key to combating this silent thief of sight is early detection followed by ongoing management of the disease.
Glaucoma consists of a group of conditions that damage the optic nerve. This nerve transmits light signals from the retina and sends the impulses to the brain, which forms the vision. Damage to the optic nerve diminishes eyesight. In the early stages of glaucoma, the decreased vision is not noticeable, but late-stage glaucoma can cause blindness.
At Wheaton Eye Clinic, glaucoma doctors perform an initial comprehensive glaucoma evaluation to:

The two most common types of glaucoma present themselves very differently. There are few or no symptoms of warning for Primary Open-Angle Glaucoma (POAG). On the other hand, some people with Angle-Closure Glaucoma (ACG) have pronounced symptoms including severe eye pain and headache, possibly nausea and vomiting, as well as blurred vision, halos around lights, sudden visual disturbances in low light and reddening of the eye. Others with ACG experience gradual loss of peripheral vision in both eyes similar to those with POAG.
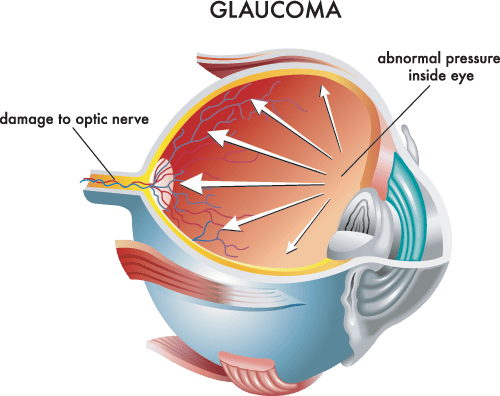
The most significant risk factors for glaucoma are increasing age and elevated internal eye pressure, which can only be detected during a doctor’s examination. People are six times more likely to get glaucoma if they are over 60 years old and the risk of glaucoma increases with age.
In addition, glaucoma is the leading cause of blindness among African Americans, who are six to eight times more likely to get glaucoma than Caucasians. African Americans should begin to have their eye pressure monitored before age 30. Hispanic populations and people of Asian descent also face an increased risk of glaucoma.
Family history can serve as an additional risk factor. Current medical findings indicate glaucoma may have a genetic link that causes members of some families to be unusually susceptible to the disease. Patients with a family history of glaucoma should be screened earlier to detect possible disease.
Medical conditions such as diabetes, heart disease or even nearsightedness can increase a person’s risk for glaucoma. Using corticosteroid medications for prolonged periods of time, especially in eye drop form, also appears to affect the risk of glaucoma. Major eye injuries can cause glaucoma to occur immediately after the injury or even years later.
Depending on the type of glaucoma being experienced, your doctor may suggest treatment involving medication and/or surgery to lower the pressure in the eye and prevent further damage to the optic nerve.
Wheaton Eye Clinic’s unparalleled commitment to excellence is evident in our continued growth. Today we provide world-class medical and surgical care to patients in six suburban locations—Wheaton, Naperville, Hinsdale, Plainfield, St. Charles, and Bartlett.
(630) 668-8250 (800) 637-1054